AN INTRODUCTION TO THE DIGESTIVE SYSTEM
• The Digestive Tract also called the gastrointestinal (GI) tract or alimentary canal, which is is a muscular tube.
• It Extends from our mouth to the anus.
• It Passes through the pharynx, esophagus, stomach, and small and large intestines.
ALIMENTARY TRAC T PARTS OF HUMA DIGESTIVE SYSTEM
The alimentary canal begins at the mouth, passes through the thorax, abdomen, and pelvis and ends at the anus. It is thus a long tube through which food passes. It has various parts that are structurally remarkably similar. The parts include:
- Mouth
- Pharynx
- Oesophagus
- Stomach
- Small intestine
- Large intestine
- Rectum and Anal canal
MOUTH
- The mouth or oral cavity is bounded by muscles and bones: anteriorly —by the lips, posteriorly — it is continuous with the oropharynx, laterally —by the muscles of the cheeks, superiorly —by the bony hard palate and muscular soft palate, inferiorly —by the muscular tongue and the soft tissues of the floor of the mouth.
- It is lined throughout with mucous membrane, consisting of stratified squamous epithelium containing small mucus-secreting glands.
- The palate forms the roof of the mouth and is divided into the anterior hard palate and the posterior soft palate. The soft palate is muscular, curves downwards from the posterior end of the hard palate, and blends with the walls of the pharynx at the sides.
- The uvula is a curved fold of muscle covered with mucous membrane, hanging down from the middle of the free border of the soft palate.
- It consists of the following important parts:
Tongue
- The tongue is a voluntary muscular structure that occupies the floor of the mouth.
- It is attached by its base to the hyoid bone and by a fold of its mucous membrane covering, called the frenulum, to the floor of the mouth.
- The superior surface consists of stratified squamous epithelium, with numerous papillae (little projections), containing nerve endings of the sense of taste, sometimes called the taste buds.
- The tongue plays an important part in:
- mastication (chewing)
- deglutition (swallowing)
- speech
- taste
Teeth
- The teeth are embedded in the alveoli or sockets of the alveolar ridges of the mandible and the maxilla.
- Each individual has two sets, the temporary or deciduous teeth, and the permanent teeth.
- At birth, the teeth of both dentitions are present in an immature form in the mandible and maxilla.
- There are 20 temporary teeth, 10 in each jaw. They begin to erupt when the child is about 6 months old, and should all be present after 24 months.
- The permanent teeth begin to replace the deciduous teeth in the 6th year of age and this dentition, consisting of 32 teeth, is usually complete by the 24th year.
Types and Functions of the teeth
The incisor and canine teeth are the cutting teeth and are used for biting off pieces of food, whereas the premolar and molar teeth, with broad, flat surfaces, are used for grinding or chewing food.
PHARYNX
- Food passes from the oral cavity into the pharynx then to the esophagus below, with which it is continuous.
- The pharynx is divided for descriptive purposes into three parts, the nasopharynx, oropharynx, and laryngopharynx.
- The nasopharynx is important in respiration. The oropharynx and laryngopharynx are passages common to both the respiratory and the digestive systems.
OESOPHAGUS
- The esophagus is about 25 cm long and about 2 cm in diameter and lies in the median plane in the thorax in front of the vertebral column behind the trachea and the heart.
- It is continuous with the pharynx above and just below the diaphragm it joins the stomach.
- The upper and lower ends of the esophagus are closed by sphincter muscles.
- The upper cricopharyngeal sphincter prevents air from passing into the esophagus during inspiration and the aspiration of oesophageal contents.
- The cardiac or lower oesophageal sphincter prevents the reflux of acid gastric contents into the esophagus.
STOMACH
- Shape : J-shaped
- Position : Epigastric, umbilical, and left hypochondriac regions of the abdominal c
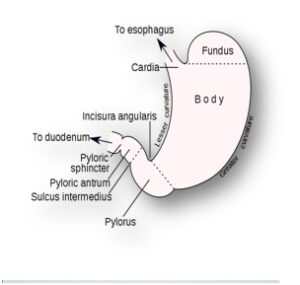
avity.
- Sphnctor : cardiac sphincter and with the duodenum at the pyloric sphincter.
- Curvatures :
lesser curvature : short, lies on the posterior surface of the stomach, and
is the downwards continuation of the posterior wall of the esophagus. Just before the pyloric sphincter, it curves upwards to complete the J shape.
Greater curvature : Where the esophagus joins the stomach the anterior region angles acutely upwards, curves downwards forming the greater curvature then slightly upwards towards the pyloric sphincter.
Parts of the Stomach : Cardiac, Fundus, Body and Pyloric.
- Stomach size varies with the volume of food it contains, which may be 1.5 liters or more in an adult.
- In the stomach, gastric muscle contraction consists of a churning movement that breaks down the bolus and mixes it with gastric juice and peristaltic waves that propel the stomach contents towards the pylorus.
- About 2 liters of gastric juice are secreted daily by special secretory glands in the mucosa.
- It consists of Water, mineral salts, mucus secreted by goblet cells in the glands and on the stomach surface, hydrochloric acid, Intrinsic factor, inactive enzyme precursors, etc.
Functions of the Stomach
- Temporary storage allowing time for the digestive enzymes, pepsins, to act.
- Chemical digestion — pepsins convert proteins to polypeptides.
- Mechanical breakdown — the three smooth muscle layers enable the stomach to act as a churn, gastric juice is added and the contents are liquefied to chime.
- Performs limited absorption of water, alcohol and some lipid-soluble drugs
- Non-specific defense against microbes — provided by hydrochloric acid in gastric juice.
- Preparation of iron for absorption further along the track — the acid environment of the stomach solubilizes iron salts, which is required before iron can be absorbed
- Production of intrinsic factor needed for absorption of vitamin B12 in the terminal ileum
- Regulation of the passage of gastric contents into the duodenum. When the chyme is sufficiently acidified and liquefied, the pyloric antrum forces small jets of gastric contents through the pyloric sphincter into the duodenum.
Mechanism of Acid Secretion
The hydrogen ion concentration in parietal cell secretions is roughly 3 million fold higher than in blood, and chloride is secreted against both a concentration and electric gradient. Thus, the ability of the partietal cell to secrete acid is dependent on active transport.
The key player in acid secretion is a H+/K+ ATPase or “proton pump” located in the cannalicular membrane.
- Hydrogen ions are generated within the parietal cell from dissociation of water. The hydroxyl ions formed in this process rapidly combine with carbon dioxide to form bicarbonate ion, a reaction cataylzed by carbonic anhydrase.
- Bicarbonate is transported out of the basolateral membrane in exchange for chloride. The outflow of bicarbonate into blood results in a slight elevation of blood pH known as the “alkaline tide”. This process serves to maintain intracellular pH in the parietal cell.
- Chloride and potassium ions are transported into the lumen of the cannaliculus by conductance channels, and such is necessary for secretion of acid.
- Hydrogen ion is pumped out of the cell, into the lumen, in exchange for potassium through the action of the proton pump; potassium is thus effectively recycled.
- Accumulation of osmotically-active hydrogen ion in the cannaliculus generates an osmotic gradient across the membrane that results in outward diffusion of water – the resulting gastric juice is 155 mM HCl and 15 mM KCl with a small amount of NaCl.
Control of Acid Secretion By Parasympathetic Nervous sytem
Parietal cells bear receptors for three stimulators of acid secretion, reflecting a triumverate of neural, paracrine and endocrine control:
- Acetylcholine (muscarinic type receptor)
- Gastrin
- Muscarininc receptor (M3)
Stimulus of hunger may be coordinated through Brain where G-Cell and vagus nerve is activated
G cell release the gastrin and vagus nerve release the Ach (Neurotransmitter).
Gastrin : further stimulate the CCK2 receptor (cholicyctokinin) on paraietal cell which stimulate Proton pump -> entry of H+ into lumen of paraietal cell .
Ach (Acetyl Choline) -> stimulate Histaminocyte -> release of histamine -> activation of H2 receptor -> Activation of proton pump -> release of H+
Muscarininc receptor (M3) : Activation of M3 receptor -> Activation of Proton pump -> release H+
SMALL INTESTINE
- The small intestine is continuous with the stomach at the pyloric sphincter and leads into the large intestine at the ileocaecal valve.
- It is a little over 5 meters long and lies in the abdominal cavity surrounded by the large intestine.
- In the small intestine, the chemical digestion of food is completed and most of the absorption of nutrients takes place.
- The small intestine comprises three main sections continuous with each other:
- The duodenum: It is about 25 cm long and curves around the head of the pancreas. Secretions from the gall bladder and pancreas are released into the duodenum through a common structure, the hepatopancreatic ampulla, and the opening into the duodenum is guarded by the hepatopancreatic sphincter (of Oddi).
- The jejunum: It is the middle section of the small intestine and is about 2 meters long.
- The ileum, or terminal section, is about 3 meters long and ends at the ileocaecal valve, which controls the flow of material from the ileum to the caecum, the first part of the large intestine, and prevents regurgitation.
- The surface area of the small intestine mucosa is greatly increased by permanent circular folds, villi, and microvilli.
- The villi are tiny finger-like projections of the mucosal layer into the intestinal lumen, about 0.5 to 1 mm long.
- Their walls consist of columnar epithelial cells, or enterocytes, with tiny microvilli (1 μm long) on their free border.
Functions of the small intestine
- The small intestine is the part of the intestines where 90% of the digestion and absorption of food occurs, the other 10% taking place in the stomach and large intestine.
- The main function of the small intestine is the absorption of nutrients and minerals from food.
LARGE INTESTINE
- It is about 5 meters long, beginning at the caecum in the right iliac fossa and terminating at the rectum and anal canal deep in the pelvis.
- Its lumen is larger than that of the small intestine. It forms an arch around the coiled-up small intestine.
- The colon is divided into the caecum, ascending colon, transverse colon, descending colon, sigmoid colon rectum, and anal canal.
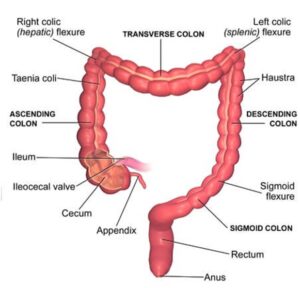
Caecum
- This is the first part of the colon. It is a dilated region which has a blind end inferiorly and is continuous with the ascending colon superiorly.
- Just below the junction of the two, the ileocaecal valve opens from the ileum.
- The vermiform appendix is a fine tube, closed at one end, which leads from the caecum. It is usually about 13 cm long and has the same structure as the walls of the colon but contains more lymphoid tissue.
The ascending colon
This passes upwards from the caecum to the level of the liver where it curves acutely to the left at the hepatic flexure to become the transverse colon.
The transverse colon
This is a loop of the colon which extends across the abdominal cavity in front of the duodenum and the stomach to the area of the spleen where it forms the splenic flexure and curves acutely downwards to become the descending colon.
The descending colon
This passes down the left side of the abdominal cavity then curves towards the midline. After it enters the true pelvis it is known as the sigmoid colon.
Sigmoid colon
This part describes an S-shaped curve in the pelvis then continues downwards to become the rectum.
Functions of the large intestine, rectum and anal canal
Absorption
- The contents of the ileum which pass through the ileocaecal valve into the caecum are fluid, even though some water has been absorbed in the small intestine.
- In the large intestine absorption of water continues until the familiar semisolid consistency of feces is achieved.
- Mineral salts, vitamins, and some drugs are also absorbed into the blood capillaries from the large intestine.
Microbial activity
- The large intestine is heavily colonized by certain types of bacteria, which synthesize vitamin K and folic acid. They include Escherichia coli, Enterobacter aerogenes, Streptococcus faecalis, andClostridium perfringens (welchii).
Defaecation
- Usually, the rectum is empty, but when a mass movement forces the contents of the sigmoid colon into the rectum the nerve endings in its walls are stimulated by a stretch.
- Defaecation involves involuntary contraction of the muscle of the rectum and relaxation of the internal anal sphincter.
- Contraction of the abdominal muscles and lowering of the diaphragm increases the intra-abdominal pressure (Valsalva’s maneuver) and so assists the process of defaecation.
Accessory Organs of digestive system
They consist of:
- Salivary glands (3 pairs)
- Pancreas
- Liver and the biliary tract.
SALIVARY GLANDS
These are present in the oral cavity and pour their secretions into the mouth.
There are three pairs: the parotid glands, the submandibular glands, and the sublingual glands.
Parotid glands
- These are situated one on each side of the face just below the external acoustic meatus.
- Each gland has a parotid duct opening into the mouth at the level of the second upper molar tooth.
Submandibular glands
- These lie one on each side of the face under the angle of the jaw.
- The two submandibular ducts open on the floor of the mouth, one on each side of the frenulum of the tongue.
Sublingual glands
- These glands lie under the mucous membrane of the floor of the mouth in front of the submandibular glands.
- They have numerous small ducts that open into the floor of the mouth.
Saliva is the combined secretions from the salivary glands and the small mucus-secreting glands of the lining of the oral cavity. About 1.5 liters of saliva is produced daily and it consists of:
- water
- mineral salts
- enzyme: salivary amylase
- mucus
- lysozyme
- immunoglobulins
- blood-clotting factors.
Functions of Salivary Glands and Saliva
- Chemical digestion of polysaccharides. Saliva contains the enzyme amylase that begins the breakdown of complex sugars, reducing them to the disaccharide maltose.
- Lubrication of food. Dry food entering the mouth is moistened and lubricated by saliva before it can be made into a bolus ready for swallowing.
- Cleansing and lubricating. An adequate flow of saliva is necessary to cleanse the mouth and keep its tissues soft, moist and pliable. It helps to prevent damage to the mucous membrane by rough or abrasive foodstuffs.
- Non-specific defense. Lysozyme, immunoglobulins and clotting factors combat invading microbes.
- The taste buds are stimulated only by chemical substances in solution. Dry foods stimulate the sense of taste only after thorough mixing with saliva.
PANCREAS
- Color : Pale grey
- Weight : 60 grams.
- Length : 12 to 15 cm
- Location: Epigastric and left hypochondriac regions of the abdominal cavity.
- It consists of a broad head, a body, and a narrow tail. The head lies in the curve of the duodenum, the body behind the stomach, and the tail lies in front of the left kidney and just reaches the spleen.
- The pancreas is both an exocrine and an endocrine gland.
The exocrine pancreas
- It consists of a large number of lobules made up of small alveoli, the walls of which consist of secretory cells.
- Each lobule is drained by a tiny duct and these unite eventually to form the pancreatic duct, which extends the whole length of the gland and opens into the duodenum.
- Just before entering the duodenum, the pancreatic duct joins the common bile duct to form the hepatopancreatic ampulla. The duodenal opening of the ampulla is controlled by the hepatopancreatic sphincter (of Oddi).
- The function of the exocrine pancreas is to produce pancreatic juice containing enzymes that digest carbohydrates, proteins, and fats.
The endocrine pancreas
- Distributed throughout the gland are groups of specialized cells called the pancreatic islets (of Langerhans).
- The islets have no ducts so the hormones diffuse directly into the blood.
- The function of the endocrine pancreas is to secrete the hormones insulin and glucagon, which are principally concerned with control of blood glucose levels.
Functions of the Pancreas
Enzymes produced by the pancreas for digestion include:
- lipase to digest fats
- amylase to digest carbohydrates
- chymotrypsin and trypsin for digesting proteins
- These enzymes travel through a series of ducts until they reach the main pancreatic duct.
- The main pancreatic duct meets the common bile duct, which carries bile from the gallbladder and liver towards the duodenum. This meeting point is called the ampulla of Vater.
- Bile from the gallbladder and enzymes from the pancreas are released into the duodenum to help digest fats, carbohydrates, and proteins so they can be absorbed by the digestive system.
Endocrine Function
As part of the endocrine system, the pancreas secretes two main hormones that are vital to regulating glucose (also known as blood sugar) level:
Insulin : lower blood glucose when levels get too high.
Glucagon : Increase blood glucose when levels get too low.
———————————————————————-
LIVER
- The liver is the largest gland in the body.
- Weight : between 1 and 2.3 kg.
- Position : upper part of the abdominal cavity occupying the greater part of the right hypochondriac region, part of the epigastric region, and extending into the left hypochondriac region.
- Lobes : The liver has four lobes. The two most obvious are the large right lobe and the smaller, wedge-shaped, left lobe. The other two, the caudate and quadrate lobes, are areas on the posterior surface.
- The lobes of the liver are made up of tiny lobules just visible to the naked eye.
- These lobules are hexagonal in outline and are formed by cubical-shaped cells, the hepatocytes, arranged in pairs of columns radiating from a central vein.
- Between two pairs of columns of cells, there are sinusoids (blood vessels with incomplete walls) containing a mixture of blood from the tiny branches of the portal vein and hepatic artery.
- Amongst the cells lining the sinusoids are hepatic macrophages (Kupffer cells) whose function is to ingest and destroy any foreign particles present in the blood flowing through the liver.
- Blood drains from the sinusoids into central or centrilobular veins. These then join with veins from other lobules, forming larger veins, until eventually, they become the hepatic veins that leave the liver and empty the inferior vena cava just below the diaphragm.
Function of the liver
- Secretion of bile.The hepatocytes synthesize the constituents of bile from the mixed arterial and venous blood in the sinusoids. These include bile salts, bile pigments, and cholesterol.
- Carbohydrate metabolism.Conversion of glucose to glycogen in the presence of insulin, and converting liver glycogen back to glucose in the presence of glucagon. These changes are important regulators of the blood glucose level.
- Fat metabolism.Desaturation of fat i.e. converts stored fat to a form in which it can be used by the tissues to provide energy.
- Protein metabolism.
-
- Deamination of amino acids removes the nitrogenous portion from the amino acids not required for the formation of new protein; urea is formed from this nitrogenous portion which is excreted in the urine.
- It also breaks down the genetic material of worn-out cells of the body to form uric acid which is excreted in the urine.
- Transamination — removes the nitrogenous portion of amino acids and attaches it to other carbohydrate molecules forming new non-essential amino acids.
- Synthesis of plasma proteins and most of the blood clotting factorsfrom the available amino acids occur in the liver.
- Breakdown of erythrocytes and defense against microbes.This is carried out by phagocytic Kupffer cells (hepatic macrophages) in the sinusoids.
- Detoxification of drugsand noxious substances. These include ethanol (alcohol) and toxins produced by microbes.
DIGESTION AND ABSORPTION
Digestion and Absorption of Carbohydrates
Digestion of carbohydrates begins in the mouth with the help of an enzyme salivary amylase. It digests the starch into maltose.
Rest of the digestion of carbohydrates occurs in small intestine with the help of the enzyme pancreatic amylase secreted by pancreas. The simplest form of carbohydrates is glucose. So all the carbohydrates consumed is finally converted into glucose for absorption.
Digestion and Absorption of Proteins
Digestion of Proteins begins in the stomach. Stomach produce an enzyme Pepsinogen. Pepsinogen is an inactive form of enzyme pepsin. Inactive form of an enzyme is known as Zymogens. Pepsinogen is converted into pepsin by Hydrochloric Acid present in the stomach. Pepsin begins the process of digestion of proteins.
Pancreas and Liver are two digestive glands that play an important role in the digestion. Pancreas secretes Trypsin and Chymotrypsin to digest proteins into small peptides. Other enzymes that participate in protein digestion are Carboxypeptidase and Proelastase. The simplest form of proteins is Amino acids in which they are absorbed by the body.
Digestion and absorption of lipids in human beings
Liver secretes bile that helps in digestion of fats (a form of lipid). The process of digestion of fats by bile is known as Emulsification of fats. Fat digestion is also promoted by lipase enzyme from the pancreas known as Pancreatic Lipase. The simplest form of fats are Fatty Acid and Glycerol. Lipase or bile breakdown fats into fatty acids and glycerol so that they can be absorbed by the body.
Digestion of Vitamins and Minerals
Digestion of Vitamins and Minerals begins in the mouth. Further digestion of vitamins and minerals occurs in the small intestine where they are also absorbed and taken to the blood stream.
GASTROINTESTINAL DISORDERS, SYMPTOMS & TREATMENT
- Celiac disease. Celiac disease is a multifactorial gastrointestinal disorder.
- Irritable Bowel Syndrome (IBS)
- Chronic Diarrhea
- Constipation
- Gastroesophageal Reflux Disease (GERD)
- Peptic Ulcer Disease
- Crohn’s Disease.
IRRITABLE BOWEL SYNDROME (IBS)
Irritable bowel syndrome (IBS) is a common disorder that affects the large intestine. Signs and symptoms include cramping, abdominal pain, bloating, gas, and diarrhea or constipation, or both. IBS is a chronic condition that you’ll need to manage long term.
Only a small number of people with IBS have severe signs and symptoms. Some people can control their symptoms by managing diet, lifestyle and stress. More-severe symptoms can be treated with medication and counseling
Symptoms
The signs and symptoms of IBS vary but are usually present for a long time. The most common include:
- Abdominal pain, cramping or bloating that is related to passing a bowel movement
- Changes in appearance of bowel movement
- Changes in how often you are having a bowel movement
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
- Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (esophagus).
- This backwash (acid reflux) can irritate the lining of your esophagus.Many people experience acid reflux from time to time. GERD is mild acid reflux that occurs at least twice a week, or moderate to severe acid reflux that occurs at least once a week.
- Most people can manage the discomfort of GERD with lifestyle changes and over-the-counter medications. But some people with GERD may need stronger medications or surgery to ease symptoms.
Symptoms
Common signs and symptoms of GERD include:
- A burning sensation in your chest (heartburn), usually after eating, which might be worse at night
- Chest pain
- Difficulty swallowing
- Regurgitation of food or sour liquid
- Sensation of a lump in your throat
PEPTIC ULCERS
Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is stomach pain.
Peptic ulcers include:
- Gastric ulcersthat occur on the inside of the stomach
- Duodenal ulcersthat occur on the inside of the upper portion of your small intestine (duodenum)
The most common causes of peptic ulcers
infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stress and spicy foods do not cause peptic ulcers. However, they can make your symptoms worse.
Symptoms
- Burning stomach pain
- Feeling of fullness, bloating or belching
- Intolerance to fatty foods
- Heartburn
- Nausea
TREATMENT
Antacids, PPIs, Ant H.Pylori
CROHN’S DISEASE
- Crohn’s disease is a type of inflammatory bowel disease (IBD).
- It causes inflammation of your digestive tract, which can lead to abdominal pain, severe diarrhea, fatigue, weight loss and malnutrition.
- Inflammation caused by Crohn’s disease can involve different areas of the digestive tract in different people. This inflammation often spreads into the deeper layers of the bowel.
- Crohn’s disease can be both painful and debilitating, and sometimes may lead to life-threatening complications.
Symptoms
- Diarrhea
- Fever
- Fatigue
- Abdominal pain and cramping
- Blood in your stool
- Mouth sores
- Reduced appetite and weight loss
- Pain or drainage near or around the anus due to inflammation from a tunnel into the skin (fistula)

